Every year, the New South Wales Food Authority (NSW Food Authority) releases their Annual Food Testing Report on the testing conducted by their primary testing provider and by other laboratories. This year’s report highlights some key findings with regards to food safety testing results and trends.
Testing is conducted for a variety of reasons including food-borne illness investigations, Food Safety Program verifications and other types of research. In the report, the NSW Food Authority breaks down the significant findings in each of these categories which provides important information for the Australian food industry.
Key facts from the report
The NSW Annual Food Testing Report provides the following facts for the period of July 2018 to June 2019:
- During this time period, there were a total of 6,431 samples submitted for testing.
- Sample types analysed included:
- meat
- seafood
- dairy
- plant products
- packaged food
- eggs
- food from retail outlets
- environmental samples
3. There were over 70 different types of tests performed. These included:
- microbiological assessment
- pH
- water activity
- allergens
- additives such as preservatives
Key findings from the report
The findings listed in the report are categorized based on different programs. The following is a breakdown of some of the key findings:
Food-borne illness investigation findings
The report states that between 2018 and 2019 there were a total of 4,010 samples (food and environmental) that were submitted for testing. These samples were submitted for testing due to food-borne illness investigations and the follow-ups for these investigations.
Increase in Salmonella Enteritidis cases
The report discusses a marked increase in the cases of Salmonella Enteritidis that has been observed since the middle of 2018. The cases have now been linked to an outbreak of Salmonella Enteritidis that was locally acquired. This a significant difference from cases of Salmonella Enteritidis in Australia in the past, with most cases typically presenting in people who had travelled overseas.
Testing was conducted and monitoring took place to determine where the outbreak was stemming from. The investigation involved taking 2,072 samples from egg production businesses and testing eggs and environmental samples. The results from the testing showed that Salmonella Enteritidis was on 13 properties that were interconnected through people, eggs and/or equipment.
The result was six food recalls at the consumer level from properties affected in NSW, and one consumer level recall in Victoria. The report states that surveillance and monitoring of NSW egg farms is slated to continue throughout 2020.
Decrease in Listeria prevalence in melons
The melon industry in Australia, particularly the rockmelon industry, has been linked to food-borne illness outbreaks of Listeria in recent years. The report states that listeriosis cases in New South Wales has actually declined sharply as of late, which is being attributed to the improved food safety measures that have been put in place in the Australian melon industry.
During the period of November 2018 and April 2019, the New South Wales Department of Primary Industries (NSW DPI) conducted food safety training workshops for rockmelon growers in NSW. NSW DPI also conducted sampling of melon harvests and packhouse environments to make sure that melon growers were following food safety protocols.
Verification findings
Concerns about Campylobacter and Salmonella on poultry
Campylobacter and Salmonella infections are both significant health concerns for Australians. In order to monitor the prevalence of these two food-borne pathogens, the raw poultry verification program gathers ongoing data on their prevalence and levels in raw poultry.
The report states that during the period of July 2018 and June 2019, samples were taken from raw poultry including 196 from whole chickens/chicken portions from processing plants, and 312 chicken portions from retail facilities. The samples were tested for the presence of Campylobacter and Salmonella.
The results for processing plants:
Salmonella
- detected in 21.4% of samples
- 9.2% of samples had quantifiable levels
Campylobacter
- detected in 86.7% of samples
- 1.5% of samples had quantifiable levels
The results for retail facilities:
Salmonella
- detected in 25.8% of samples
- 1.7% of samples had quantifiable levels
Campylobacter
- detected in 89.9% of samples
- 6.4% of samples had quantifiable levels
Research findings
Investigating algal biotoxins in wild harvest shellfish
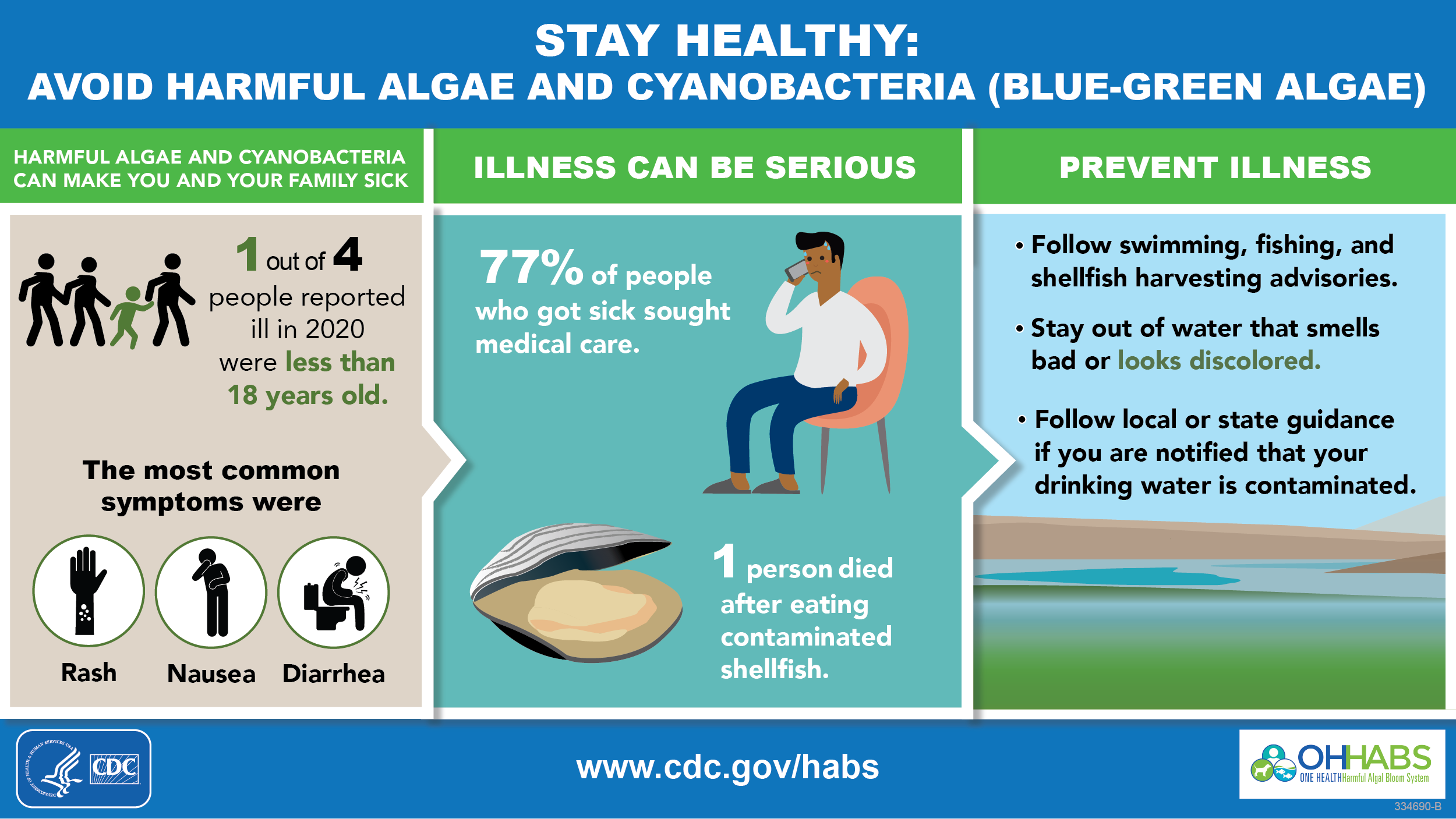
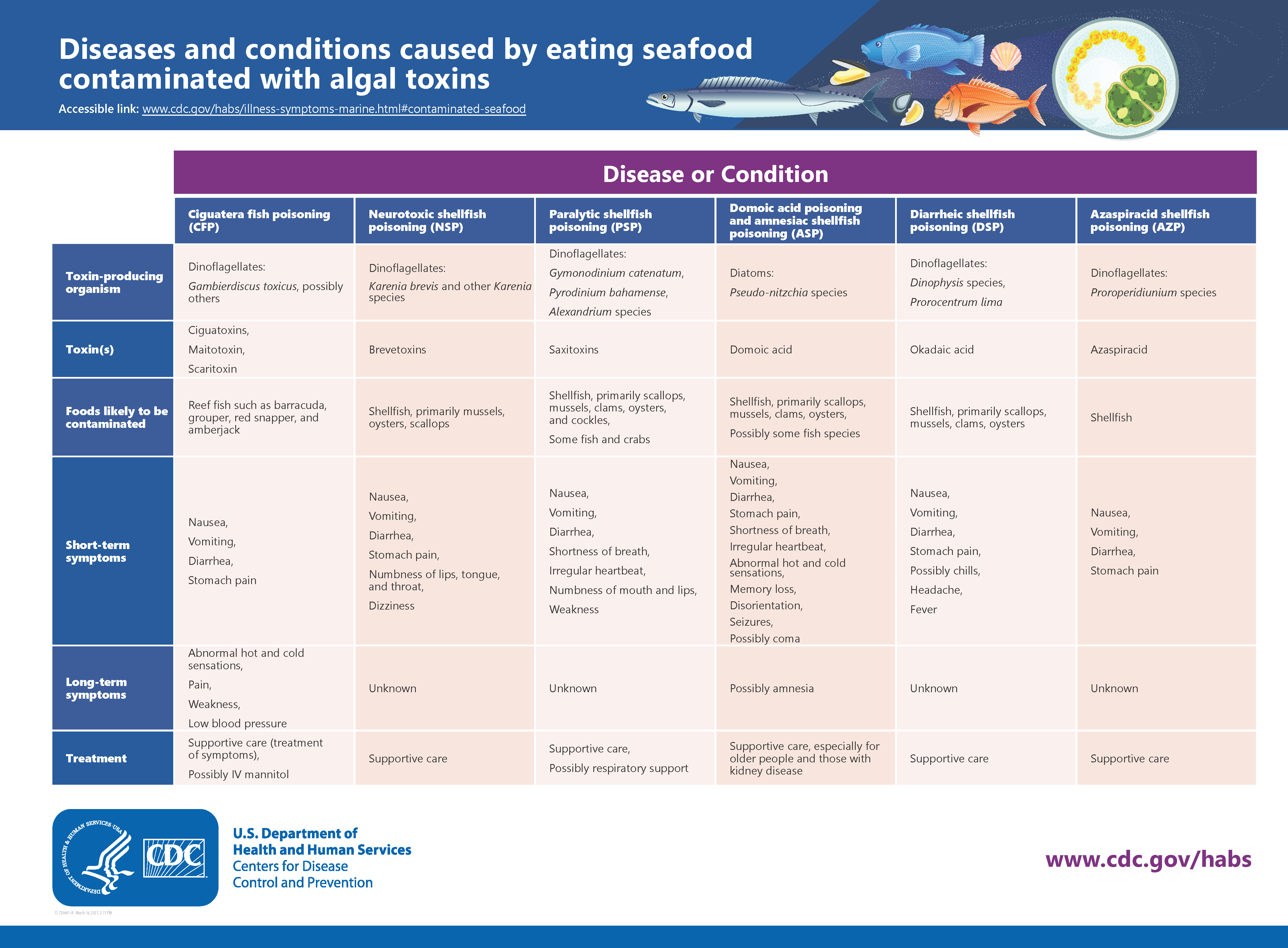
There are other types of food-borne pathogens that are not as well known as Listeria, Salmonella or Campylobacter. The report touches on how some algae produce toxic compounds that can then accumulate in certain types of fish, particularly filter-feeding bivalve shellfish. The concern is that the toxic compounds can be harmful to humans if they are consumed by eating the shellfish.
The NSW Food Authority conducted testing between 2018 and 2019 which involved taking samples from pipis which are a type of shellfish group. There were 76 samples taken and they were tested for three different types of algae toxin groups which were amnesic shellfish toxins, paralytic shellfish toxins and diarrhetic shellfish toxins. The results revealed that diarrhetic shellfish toxins were detected in 13 of the 76 samples.
The NSW Food Authority will continue to investigate the health concerns around algae toxins in harvest shellfish in the 2019-2020 fiscal year.