Ciguatera poisoning (CP) is caused by consumption of fish that have accumulated ciguatoxins in their flesh. CP is endemic in tropical and subtropical regions, particularly in the Pacific and Indian Oceans and the Caribbean Sea. Isolated outbreaks have occurred sporadically in Europe but with an increasing frequency in temperate areas like the Canary Islands, Spain.
CP is not under routine surveillance in the European Union (EU), but unexpected, potentially serious cross-border biological threats to health are monitored by ECDC [1]. Cases are usually not notified in national surveillance systems but may be reported to national poisoning centres.
Ciguatoxins
Ciguatoxins (CTXs) are temperature-stable, so they are not destroyed by cooking or by freezing the fish. Furthermore, the toxins are colourless, odourless, and flavourless, which make it impossible to taste or smell them [2,3].
Transmission
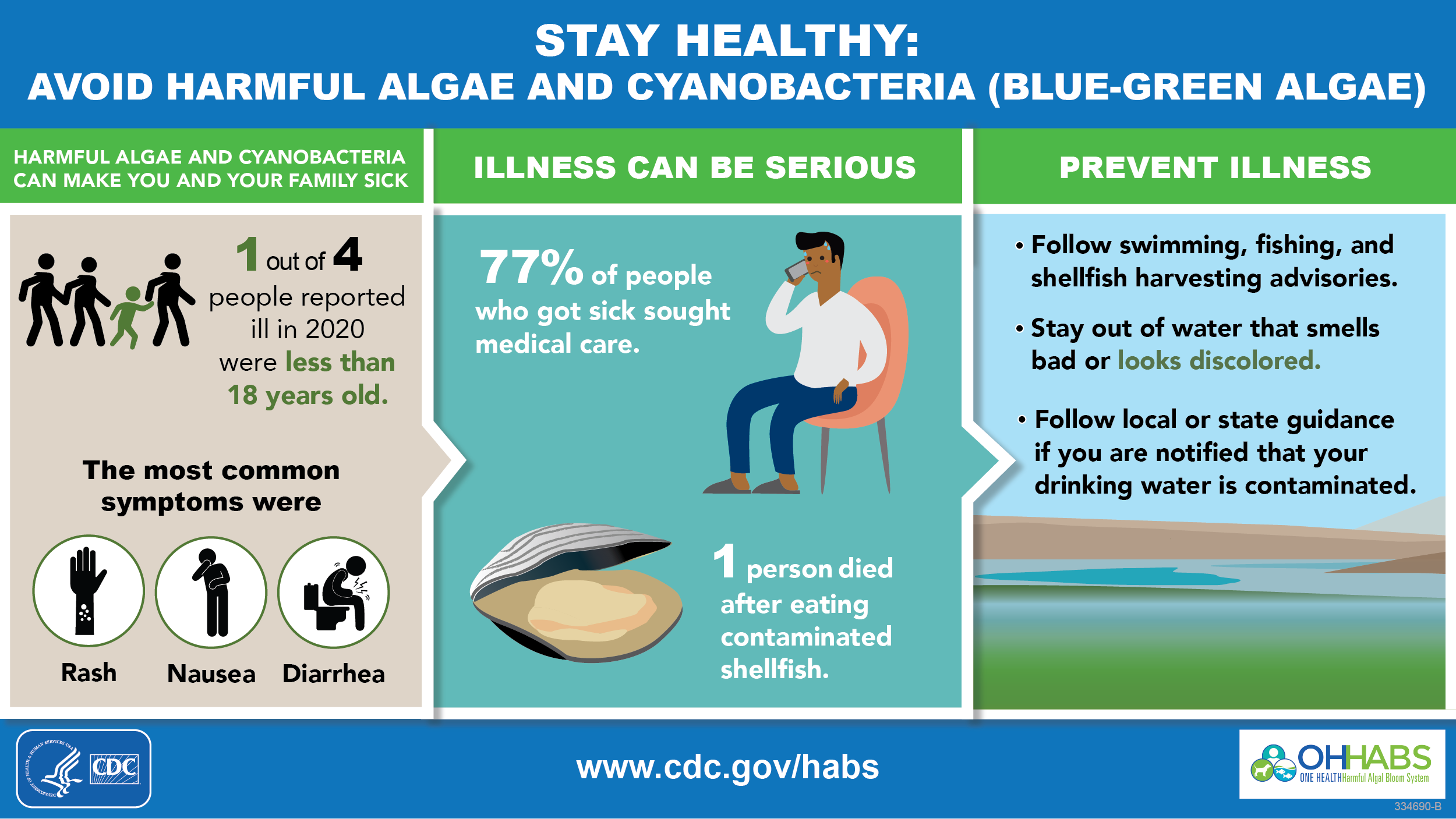
CP is caused by the consumption of herbivorous fish that feed on toxic microalgae (Gambierdiscus spp. and Fukuyoa spp.), which are attached to macrophytes or dead corals, and from carnivorous fish that have consumed toxic herbivorous fish [3,4].
Over 400 known fish species from tropical and subtropical waters have been classified as potential carriers of CTXs. Examples of the fish most frequently associated with cases of CP include barracuda, grouper, amberjack, snapper, moray eel, hogfish, mackerel, surgeonfish, and parrotfish. Greater severity of illness is associated with eating fish head or organs. It is therefore advisable to avoid consuming visceral organs, roe (fish eggs), and carcasses (e.g. heads, eyes, and bones) of these fish species [4-6].
Person-to-person transmission of CTXs is extremely rare, but transmission of toxin from mother to child during breastfeeding or across the placenta, as well as during sexual intercourse, has been described [6-10].
Clinical features and sequelae
Intoxication of humans occurs via consumption of fish containing CTXs. In humans, CTXs activate voltage-gated sodium channels in cell membranes, increasing sodium ion permeability and depolarizing the nerve cell. Clinical presentation varies according to the individual characteristics and the geographical origin of the CTXs. Gastrointestinal symptoms can precede or accompany neurological symptoms, which usually appear two to 48 hours after eating the contaminated fish. Symptoms can include nausea, vomiting, diarrhoea, abdominal cramps, paraesthesia of lips, tongue and extremities, cold allodynia (burning pain caused by a normally innocuous cold stimulus), a metallic taste in the mouth, arthralgia, myalgia, pruritus without urticaria or erythema, muscle weakness, blurred vision, painful intercourse, hypotension, and bradycardia [4,8,11].
Cold allodynia is characteristic of CP, although it is not present in all patients. Neurological symptoms usually resolve within weeks, although some symptoms can last for months. Recurrent symptoms can occur following the ingestion of certain food or beverages such as alcohol, nuts, or non-toxic fish. CP is rarely fatal, but death can occur in severe cases due to severe dehydration, cardiovascular shock, or respiratory failure [4,8,11].