Abstract and Introduction
Introduction
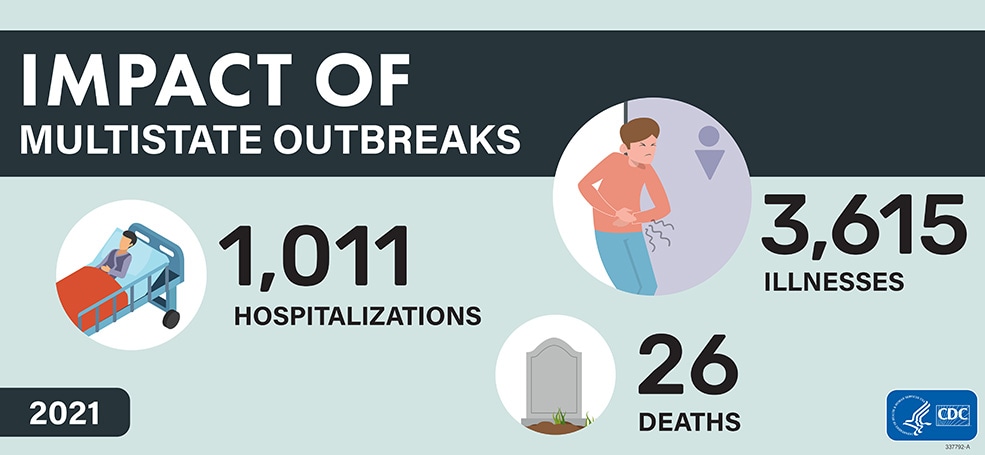
Each year, infections from major foodborne pathogens are responsible for an estimated 9.4 million illnesses, 56,000 hospitalizations, and 1,350 deaths in the United States.[1] To evaluate progress toward prevention of enteric infections in the United States, the Foodborne Diseases Active Surveillance Network (FoodNet) conducts surveillance for laboratory-diagnosed infections caused by eight pathogens transmitted commonly through food at 10 U.S. sites. During 2020–2021, FoodNet detected decreases in many infections that were due to behavioral modifications, public health interventions, and changes in health care–seeking and testing practices during the COVID-19 pandemic. This report presents preliminary estimates of pathogen-specific annual incidences during 2022, compared with average annual incidences during 2016–2018, the reference period for the U.S. Department of Health and Human Services’ Healthy People 2030 targets.[2] Many pandemic interventions ended by 2022, resulting in a resumption of outbreaks, international travel, and other factors leading to enteric infections. During 2022, annual incidences of illnesses caused by the pathogens Campylobacter, Salmonella, Shigella, and Listeria were similar to average annual incidences during 2016–2018; however, incidences of Shiga toxin-producing Escherichia coli (STEC), Yersinia, Vibrio, and Cyclospora illnesses were higher. Increasing culture-independent diagnostic test (CIDT) usage likely contributed to increased detection by identifying infections that would have remained undetected before widespread CIDT usage. Reducing pathogen contamination during poultry slaughter and processing of leafy greens requires collaboration among food growers and processors, retail stores, restaurants, and regulators.