Archives
-
Join 343 other subscribers
KSWFoodWorld
Blog Stats
- 431,447 Views
Category Archives: Algal Toxin
Research – Microbiological and Toxicological Investigations on Bivalve Molluscs Farmed in Sicily
Bivalves can concentrate biological and chemical pollutants, causing foodborne outbreaks whose occurrence is increasing, due to climatic and anthropic factors that are difficult to reverse, hence the need for improved surveillance. This study aimed to evaluate the hygienic qualities of bivalves sampled along the production and distribution chain in Sicily and collect useful data for consumer safety. Bacteriological and molecular analyses were performed on 254 samples of bivalves for the detection of enteropathogenic Vibrio, Arcobacter spp., Aeromonas spp., Salmonella spp., and beta-glucuronidase-positive Escherichia coli. A total of 96 out of 254 samples, collected in the production areas, were processed for algal biotoxins and heavy metals detection. Bacterial and algal contaminations were also assessed for 21 samples of water from aquaculture implants. Vibrio spp., Arcobacter spp., Aeromonas hydrophila, Salmonella spp., and Escherichia coli were detected in 106/254, 79/254, 12/254, 16/254, and 95/254 molluscs, respectively. A total of 10/96 bivalves tested positive for algal biotoxins, and metals were under the legal limit. V. alginolyticus, A. butzleri, and E. coli were detected in 5, 3, and 3 water samples, respectively. Alexandrium minutum, Dinophysis acuminata, Lingulodinium polyedra, and Pseudonitzschia spp. were detected in water samples collected with the biotoxin-containing molluscs. Traces of yessotoxins were detected in molluscs from water samples containing the corresponding producing algae. Despite the strict regulation by the European Commission over shellfish supply chain monitoring, our analyses highlighted the need for efficiency improvement.
RASFF Alert- Lipophilic Toxin – Mussels
Presence of lipophilic toxin detected in mussels from France in Switzerland
Posted in Algal Toxin, food contamination, food handler, Food Hazard, Food Hygiene, Food Inspections, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Testing, Food Poisoning, Food Quality, food recall, Food Safety, Food Safety Alert, Food Safety Management, Food Safety Regulations, Food Testing, Food Toxin, Lipophilic Marine Biotoxin, Marine Biotoxin, Toxin
New Zealand – Shellfish biotoxin alert – North Island
North Island warning
| Reason for alert | Paralytic Shellfish Poisoning (PSP) |
| Date warning issued | 10 May 2023 |
| Affected area | Western side of the Firth of Thames. |
| Shellfish affected | Mussels, oysters, tuatua, pipi, toheroa, cockles, scallops, catseyes, kina (sea urchin) and all other bivalve shellfish.
Note, cooking shellfish does not remove the toxin. Pāua, crab and crayfish may still be eaten if the gut has been completely removed prior to cooking, as toxins accumulate in the gut. If the gut is not removed its contents could contaminate the meat during the cooking process. |
| Symptoms | Symptoms typically appear between 10 minutes and 3 hours after ingestion and may include:
|
| Other information | Paralytic shellfish toxins have been detected in shellfish from the Kaipara Harbour at levels over the safe limit of 0.8mg/kg set by MPI. Ongoing testing will continue and any changes will be communicated accordingly. |
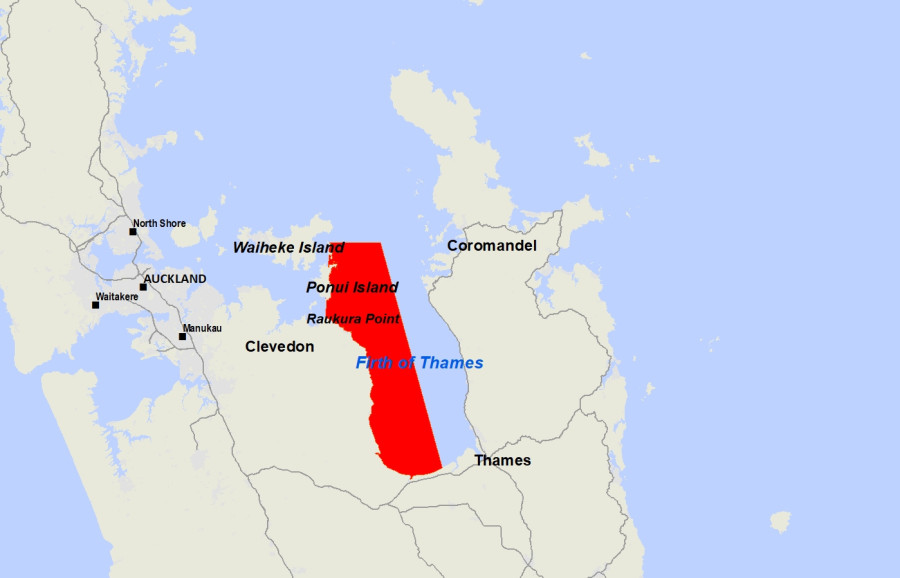
Map of the affected area
Public warnings about toxic shellfish
We test shellfish and seawater for toxic algae every week from popular shellfish gathering areas around New Zealand. If the shellfish are not safe to eat, we issue public health warnings and put up signs at affected beaches.
Posted in Algal Toxin, Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Lipophilic Marine Biotoxin, Marine Biotoxin, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, MPI, paralytic shellfish poisoning, PSP
Vanuatu: Dozens of ciguatera cases reported since the beginning of the year
The Vanuatu Ministry of Health reports that from January 1 to March 19, 27 ciguatera fish poisoning cases were recorded, all were clinically diagnosed.
The cases were distributed as follows: Seventeen (17) cases from Efate, 6 cases from Maewo, 2 cases from Ambrym, 1 from Ambae, 1 from Pentecost and 1 from Santo.
No deaths have been recorded.
From the cases reported, 69% of the cases consumed reef fish – not specified, 16 consumed Snapper and 15% consumed grouper.
More than 400 species of fish, including barracuda, black grouper, blackfin snapper, cubera snapper, dog snapper, greater amberjack, hogfish, horse-eye jack, king mackerel, and yellowfin grouper have been implicated in this food borne illness that’s relatively common in several areas of the world.
Posted in Algal Toxin, Ciguatera, Ciguatera Poisoning, Decontamination Microbial, Dinoflagellates, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Toxin, Marine Biotoxin, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Toxin
New Zealand – Shellfish biotoxin alert – Firth of Thames
New Zealand Food Safety today issued a public health warning advising the public not to collect or consume shellfish harvested from the entire Firth of Thames area up to a line from Raukura Point across to Deadmans Point.
Routine tests on shellfish samples taken from this region have shown levels of Paralytic Shellfish Poisoning (PSP) toxins above the safe limit of 0.8 mg/kg set by New Zealand Food Safety. Anyone eating shellfish from this area is potentially at risk of illness.
Mussels, oysters, tuatua, pipi, toheroa, cockles, scallops, catseyes, kina (sea urchin) and all other bivalve shellfish should not be eaten.
Note: cooking shellfish does not remove the toxin.
Pāua, crab and crayfish may still be eaten if the gut has been completely removed prior to cooking, as toxins accumulate in the gut. If the gut is not removed its contents could contaminate the meat during the cooking process.
Symptoms typically appear between 10 minutes and 3 hours after ingestion and may include:
- numbness and a tingling (prickly feeling) around the mouth, face, and extremities (hands and feet)
- difficulty swallowing or breathing
- dizziness
- headache
- nausea
- vomiting
- diarrhoea
- paralysis and respiratory failure and in severe cases, death.
If anyone becomes ill after eating shellfish from an area where a public health warning has been issued, phone Healthline for advice on 0800 61 11 16, or seek medical attention immediately. You are also advised to contact your nearest public health unit and keep any leftover shellfish in case it can be tested.
Monitoring of toxin levels will continue and any changes will be communicated accordingly. Commercially harvested shellfish – sold in shops and supermarkets, or exported – is subject to strict water and flesh monitoring programmes by MPI to ensure they are safe to eat.
Posted in Algal Toxin, Food Microbiology, Food Microbiology Blog, Food Microbiology Testing, Food Safety Alert, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, paralytic shellfish poisoning, PSP, Shellfish, shellfish toxin
Research – The monitoring program for algal toxins in shellfish 2021
In general, less poisonous shells were detected during the covid-19 years 2020 and 2021 than in the three previous years. We cannot determine whether this is due to fewer samples or less blooms of toxic algal plankton.
In 2021, a total of 723 shell samples were taken and analyzed for various toxins; 384 samples from the Norwegian Food Safety Authority’s annual monitoring program (including the Mussel Alert) and 339 samples from the producers’ own control samples.
The number of samples from the industry was somewhat fewer in 2021 because demand for shells was lower due to covid-19 with closed restaurants and hotels.
On the monitoring of algal toxins in shellfish
The Norwegian coast is monitored throughout the year for marine algal toxins in shells in connection with commercial harvesting and trade in addition to the Mussel Alert.
The shell samples are analyzed for both the fat-soluble toxins DSP (OA group), AZA, YTX and PTX and the water-soluble toxins with the neurotoxin PSP (STX group), and for the amnesia toxin ASP (DA group).
| What did we investigate? | Mostly mussels, but also some scallops, flat oysters, Pacific oysters, cockles, knife clams, O-clams, carpet clams, sand clams, circle clams, king snails and sea urchins |
| Time range: | 2021 |
| What were we looking for? | The algae toxins DSP, YTX, PTX and AZA, PSP and ASP. |
| What did we find? | Around 98 per cent of all submitted mussels were below the limit value for DSP (OA group).
For PSP (STX group) around 95 per cent were below the limit value, while around 99 per cent were below the limit value for ASP. For the toxin groups YTX, PTX and AZA, all samples were below given limit values. Mussels: Had the most detections of DSP and PSP above the limit value, but ASP was also detected above the limit value Scallops : PSP and ASP were detected above the limit value Flat oysters : PSP was detected above the limit value in Western Norway for a period in April PSP : As in previous years, was mainly detected in the spring and early summer. DSP : The detections above the limit value were distributed throughout the year from April to October with a peak in September. This is consistent with previous years where DSP mainly performs in late summer and autumn. |
Posted in Algal Blooms, Algal Toxin, ASP, Azaspiracid Toxin, Decontamination Microbial, Diarrhoeic Shellfish Poisoning, DSP, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, paralytic shellfish poisoning, PSP
Research – Illnesses Linked to Harmful Algal Blooms
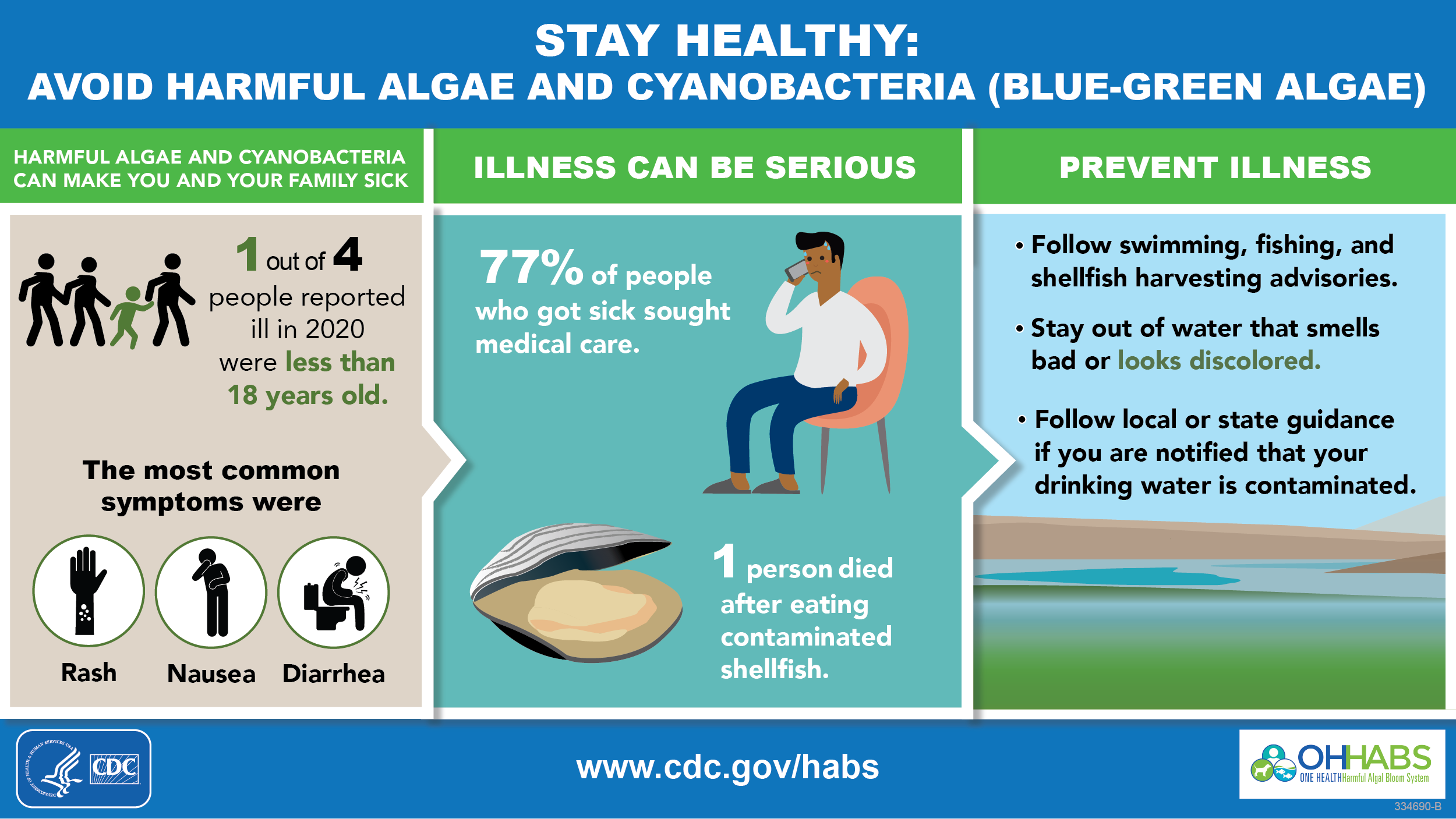
Highlight
- Thirteen states reported 227 harmful algal blooms (HABs) that resulted in a total of 95 human illnesses and at least 1,170 animal illnesses.
- The first human death reported in OHHABS was associated with paralytic shellfish poisoning.
- A HAB event in September killed at least 1,000 fish (carp).
- 22 human illnesses (23%) were associated with national parks, with 21 illnesses attributed to a single HAB event.
Background
Harmful algal blooms (HABs) that result from the rapid growth of algae or cyanobacteria (sometimes referred to as blue-green algae) in natural waterbodies can harm people, animals, or the environment. HAB events of public health concern are primarily caused by microalgae called diatoms and dinoflagellates, cyanobacteria, and the toxins they can produce. HAB events, which can be intensified by factors such as nutrient pollution and warmer water temperature, can have public health, environmental, and economic impacts.
HABs are a One Health issue—they affect the health of people, animals, and our shared environment. One Health is a collaborative and multi-sectoral approach that involves engagement across disciplines including public health, animal health, and environmental health. Using a One Health approach, CDC collects data about HAB events and associated human or animal illnesses through the One Health Harmful Algal Bloom System (OHHABS) to inform public health prevention efforts.
Within the context of OHHABS, the term HAB event describes the identification of a bloom or the detection of HAB toxins in water or food (i.e., absent a visual bloom). Human illnesses are reported individually. Animal illnesses are reported as single cases of illness or in groups, such as flocks of birds. The reporting system can link HAB event data with human or animal illness data. OHHABS uses standard definitions [PDF – 3 pages] to classify HAB events as suspected or confirmed and human or animal illness as suspected, probable, or confirmed.
OHHABS is available for voluntary reporting by public health agencies and their designated environmental health or animal health partners in the United States, District of Columbia, Federated States of Micronesia, Guam, Marshall Islands, Northern Mariana Islands, Palau, Puerto Rico, and U.S. Virgin Islands. Public health agencies use standard forms to report HAB events, human cases of illness, and animal cases of illness to OHHABS. Public health agencies do not need to submit all three types of forms to participate.
Data collected for HAB events include general information (e.g., observation date), geographic information, water body characteristics (e.g., salinity), observational characteristics (e.g., water color, scum), and laboratory testing. Data collected for cases of illness include general demographic characteristics, exposure information, signs and symptoms, medical care, and health outcomes. OHHABS is a dynamic electronic reporting system; data within individual reports are subject to change over time. Data included in this report are from a specific point in time.
Posted in Algal Blooms, Algal Toxin, Food Illness, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Foodborne Illness, Illness, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk
RASFF Alerts – Marine Lipophilic – Biotoxin- Algal Toxin
Lipophilic biotoxins in cockles from Portugal in Spain
Posted in Algal Toxin, food contamination, food handler, Food Hazard, Food Hygiene, Food Inspections, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Testing, Food Poisoning, food recall, Food Safety, Food Safety Alert, Food Safety Management, Food Testing, Food Toxin, Lipophilic Marine Biotoxin
Norway -Crab shells in Agder: DSP below limit value
On 22 September, the Norwegian Food Safety Authority received a response to new samples of crabs in Agder. The random samples show that diarrhea toxin (DSP) in the crabs is now below the limit value, but there is no guarantee that all crabs in the area are below the danger limit. The Norwegian Food Safety Authority recommends following the mussel warning, as the crab likes to eat mussels.
Earlier in September, the Norwegian Food Safety Authority found high concentrations of the algae poison DSP (Diarrhetic Shellfish Poisoning) in crab from Agder, and thus warned people to eat the contents of crab shells.
DSP is one of the most common types of mussel poisoning in Norway. Once the crab has eaten mussels with DSP, the crab becomes poisonous to people who eat it. DSP causes diarrhoea, nausea, vomiting and abdominal pain. It takes from half an hour to a few hours from the time you eat until you get sick. The symptoms disappear by themselves after 2-3 days.
Since the beginning of July this year, high levels of the algal toxin DSP have been detected in mussels along the Sørland coast and in Agder.
Posted in Algal Toxin, Diarrhoeic Shellfish Poisoning, DSP, food contamination, food handler, Food Hazard, Food Hygiene, Food Inspections, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Testing, Food Poisoning, food recall, Food Safety, Food Safety Alert, Food Safety Management, Food Testing, Food Toxin, Lipophilic Marine Biotoxin, Marine Biotoxin, Toxin
New Zealand – Public health warning for shellfish reduced for West Coast, North Island – PSP Toxins
New Zealand Food Safety today reduced a public health warning against collecting shellfish in the Waikato and Taranaki region. The public health warning now extends from Albatross Point south to Oakura Beach and no longer applies to Kawhia and Aotea Harbours. More testing is being undertaken to determine the levels of paralytic shellfish toxins in the affected area.
Routine tests on shellfish samples taken from the Aotea/Kawhia Harbour area have shown levels of Paralytic Shellfish Poisoning (PSP) toxins are now within the safe limit of 0.8 mg/kg set by New Zealand Food Safety.
Mussels, oysters, tuatua, pipi, toheroa, cockles, scallops, catseyes, kina (sea urchin), and all other bivalve shellfish should not be eaten.
Note, cooking shellfish does not remove the toxin.
Pāua, crab, and crayfish may still be eaten if the gut has been completely removed prior to cooking, as toxins accumulate in the gut. If the gut is not removed, its contents could contaminate the meat during the cooking process.
Symptoms typically appear between 10 minutes and 3 hours after ingestion and may include:
- numbness and a tingling (prickly feeling) around the mouth, face, and extremities (hands and feet)
- difficulty swallowing or breathing
- dizziness
- headache
- nausea
- vomiting
- diarrhoea
- paralysis and respiratory failure and in severe cases, death.
If anyone becomes ill after eating shellfish from an area where a public health warning has been issued, phone Healthline for advice on 0800 61 11 16, or seek medical attention immediately. You are also advised to contact your nearest public health unit and keep any leftover shellfish in case it can be tested.
Monitoring of toxin levels will continue and any changes will be communicated accordingly. Commercially harvested shellfish – sold in shops and supermarkets, or exported – is subject to strict water and flesh monitoring programmes by MPI to ensure they are safe to eat.
Posted in Algal Toxin, Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Toxin, Lipophilic Marine Biotoxin, Marine Biotoxin, microbial contamination, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, MPI, paralytic shellfish poisoning, PSP


