Archives
-
Join 343 other subscribers
KSWFoodWorld
Blog Stats
- 429,590 Views
Category Archives: Pathogen
Research – Presence of Foodborne Bacteria in Wild Boar and Wild Boar Meat—A Literature Survey for the Period 2012–2022
The wild boar is an abundant game species with high reproduction rates. The management of the wild boar population by hunting contributes to the meat supply and can help to avoid a spillover of transmissible animal diseases to domestic pigs, thus compromising food security. By the same token, wild boar can carry foodborne zoonotic pathogens, impacting food safety. We reviewed literature from 2012–2022 on biological hazards, which are considered in European Union legislation and in international standards on animal health. We identified 15 viral, 10 bacterial, and 5 parasitic agents and selected those nine bacteria that are zoonotic and can be transmitted to humans via food. The prevalence of Campylobacter, Listeria monocytogenes, Salmonella, Shiga toxin-producing E. coli, and Yersinia enterocolitica on muscle surfaces or in muscle tissues of wild boar varied from 0 to ca. 70%. One experimental study reported the transmission and survival of Mycobacterium on wild boar meat. Brucella, Coxiella burnetii, Listeria monocytogenes, and Mycobacteria have been isolated from the liver and spleen. For Brucella, studies stressed the occupational exposure risk, but no indication of meat-borne transmission was evident. Furthermore, the transmission of C. burnetii is most likely via vectors (i.e., ticks). In the absence of more detailed data for the European Union, it is advisable to focus on the efficacy of current game meat inspection and food safety management systems.
Posted in Brucella melitensis, Brucellosis, Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, Listeria, Listeria monocytogenes, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Mycobacterium, Pathogen, pathogenic, STEC, STEC E.coli, Yersinia, Zoonosis
Research – Contribution of MALDI-TOF-MS-based principal component analysis for distinguishing foodborne pathogens
Abstract
Foodborne diseases are important to determine bacteria in strain level, which are analyzed by library-based devices and bioinformatics-enabled. The aim of this study was to investigate the contribution of principal component analysis (PCA) with matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOF-MS) to distinguish according to the differences of bacterial strains as rapidly screening of foodborne bacteria. The MALDI-TOF-MS-based PCA analysis was used for differentiating bacterial strains isolated from ready-to-eat foods. According to the results of PCA analysis, the percentages of distance and proximity between species were evaluated by composite correlation indexes (CCI). Bacillus cereus were detected in burghul salad (BC1) and macaroni salad (BC2) taken from the SB2-snack bar, and the similarity rate was determined as 97%. Three other B. cereus bacteria (BC3, BC4, and BC5) in the same cluster were also isolated from salads collected from SB4-snack bar. The similarity of Klebsiella pneumoniae bacteria, which have the codes KP1 and KP2, isolated from macaroni salad and burghul salad taken from the SB2 snack bar respectively were 96%. Additionally, the CCI values of two E. coli strains in burghul (EC1) salad and Russian salad (EC2) in the same sampling point (SB1) were determined as 97%. In conclusion, this analysis with MALDI-TOF-MS based PCA has revealed the relationships between bacteria genera and species, beyond just the identification of bacteria and the rapid screening of bacteria in perishable foodstuffs. Similarities between bacterial strains identified for different samples from the same sampling point suggested that there were not adequate hygiene rules and storage requirements were not followed.
Posted in Bacillus cereus, Decontamination Microbial, E.coli, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, Klebsiella, Malditof, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Pathogen, pathogenic
Research – Listeria in Food: Prevalence and Control
Listeria monocytogenes is a foodborne pathogen characterized by its psychrotrophic and ubiquitous nature as well as its ability to survive and proliferate in a wide range of harsh environments and foods. These features make the pathogen a primary concern in the food industry, especially in the cold chain of ready-to-eat (RTE) food products. Although the incidence of listeriosis is low compared to other foodborne illnesses (e.g., salmonellosis), its high hospitalization and case fatality rates, mainly in high-risk population groups, pose a significant threat to public health.
The prevalence of L. monocytogenes has been reduced in many food categories over the last two decades, especially in meat and meat products, due to the application of improved control measures. As highlighted by Abdeen et al. [1] in this Special Issue, the application of suitable control measures along the food chain to reduce pathogen levels and prevent product recontamination together with the continuous training of food handlers are key to reduce the pathogen incidence. They found that the prevalence of L. monocytogenes in different RTE food products from Egypt was higher compared to other Listeria species. In addition, the pathogen isolates carried multiple virulence-related genes (hlyA, iap, and actA) and showed phenotypic resistance to six antibiotics. This highlights the importance of monitoring the emergence of resistant and virulent strains.
The presence of persister cells and biofilms in food processing environments also requires attention. In the study by Panebianco et al. [2], the effectiveness of gaseous ozone against the biofilm of L. monocytogenes isolates from different sources was evaluated. They concluded that ozone gas was not sufficient to completely counteract the pathogen biofilm, but it may be useful as an additional tool to improve the existing sanitization procedures in food processing environments. On the other hand, the development of innovative control approaches with reduced environmental impact is necessary to offer consumers more natural solutions and chemical-free products. In this context, van Gijtenbeek et al. [3] assessed the bioprotective potential of the Lacticaseibacillus rhamnosus strain Lrh-FQ to inhibit the growth of L. monocytogenes in creamed cottage cheese. The mechanism underlying the pathogen inhibition was based on competitive exclusion through the depletion of manganese content in the food matrix by Lrh-FQ.
A rapid and accurate detection of L. monocytogenes in food is also important to avoid sanitary and economic problems. Different methods are currently used for the detection of L. monocytogenes in food, such as conventional methods based on ISO standards using chromogenic media or biochemical tests. Alternative methods that reduce timing in pathogen detection are needed to prevent its dissemination through the food chain. In this context, Estévez et al. [4] evaluated the Vitek Immuno Diagnostic Assay System (VIDAS) to detect and count L. monocytogenes in various food items, demonstrating that VIDAS showed high efficiency and was not influenced by the food matrix or interfering microorganisms.
Predictive microbiology is a useful tool to estimate food shelf life and assist regulators in decision making. The development and/or validation of predictive models in real food products and the use of pathogen isolates from particular foods are essential to obtain accurate predictions of food systems. In this regard, Posada-Izquierdo et al. [5] modeled the effect of salt concentration on autochthonous isolated L. monocytogenes strains in an artisanal fresh cheese. Finally, Bolívar et al. [6] quantified and modeled the growth dynamics of six L. monocytogenes strains isolated from different fish products in salmon pâté. Both studies have demonstrated the growth potential of the pathogen under all tested conditions, providing interesting data about its kinetic behavior in RTE food products with significant consumption and commercial value.
The prevention of listeriosis relies on a comprehensive approach from farm to fork. This Special Issue of Foods, including five original articles and one short research communication, provides a deep understanding on the prevalence and genetic characteristics of L. monocytogenes, its growth dynamics in different RTE food products by suitable predictive tools, as well as the efficacy of different detection and control approaches. This insight can support the development of new and robust risk management strategies aimed at reducing the risk of listeriosis.
Posted in Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, Listeria, Listeria monocytogenes, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Pathogen, pathogenic
Research – Microbiological Quality and Safety of Fresh Turkey Meat at Retail Level, Including the Presence of ESBL-Producing Enterobacteriaceae and Methicillin-Resistant S. aureus
Abstract
The aim of this work was to study the microbiological safety and quality of marketed fresh turkey meat, with special emphasis on methicillin-resistant S. aureus, ESBL-producing E. coli, and K. pneumoniae. A total of 51 fresh turkey meat samples were collected at retail level in Spain. Mesophile, Pseudomonas spp., enterococci, Enterobacteriaceae, and staphylococci counts were 5.10 ± 1.36, 3.17 ± 0.87, 2.03 ± 0.58, 3.18 ± 1.00, and 2.52 ± 0.96 log CFU/g, respectively. Neither Campylobacter spp. nor Clostridium perfringens was detected in any sample. ESBL-producing K. pneumoniae and E. coli were detected in 22 (43.14%), and three (5.88%) samples, respectively, all of which were multi-resistant. Resistance to antimicrobials of category A (monobactams, and glycilcyclines) and category B (cephalosporins of third or fourth generation, polymixins, and quinolones), according to the European Medicine Agency classification, was found among the Enterobacteriaceae isolates. S. aureus and methicillin-resistant S. aureus were detected in nine (17.65%) and four samples (7.84%), respectively. Resistance to antimicrobials of category A (mupirocin, linezolid, rifampicin, and vancomycin) and category B (cephalosporins of third- or fourth generation) was found among S. aureus, coagulase-negative staphylococci, and M. caseolyticus isolates.
Posted in Enterococcus, ESBL, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, MRSA, Pathogen, Staphylococcal Toxin, Staphylococcus aureus
Research – Current Perspectives on Viable but Non-Culturable Foodborne Pathogenic Bacteria: A Review
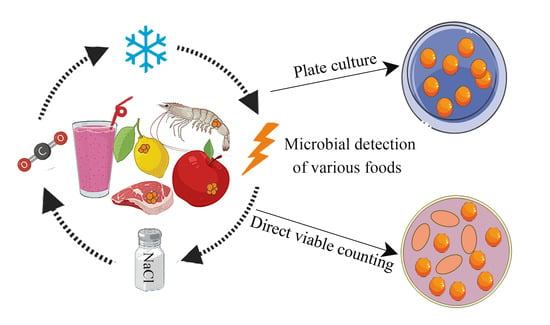
Abstract
Foodborne diseases caused by foodborne pathogens pose risks to food safety. Effective detection and efficient inactivation of pathogenic bacteria has always been a research hotspot in the field of food safety. Complicating these goals, bacteria can be induced to adopt a viable but non-culturable (VBNC) state under adverse external environmental stresses. When in the VBNC state, pathogens cannot form visible colonies during traditional culture but remain metabolically active and toxic. The resulting false negative results in growth-related assays can jeopardize food safety. This review summarizes the latest research on VBNC foodborne pathogens, including induction conditions, detection methods, mechanism of VBNC formation, and possible control strategies. It is hoped that this review can provide ideas and methods for future research on VBNC foodborne pathogenic bacteria.
Posted in Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Pathogen, pathogenic, Research
Research – Human Pathogens in Primary Production Systems
Human pathogenic micro-organisms can contaminate plants. Plants whose products can be consumed freshly or after minimal processing are of specific concern. It is under debate whether contaminations only occur at harvest or the after harvest processing of crops, or if they can already occur at the primary plant production stages.
Plants may be considered as secondary habitats for human pathogens [1], and, although they do not possess the full capacity to invade and colonize internal tissues of plants, like plant pathogens and endophytes do [2], they are still capable of maintaining themselves in the neighborhood of, and even inside, plants [3], and to proliferate in these ecosystems. Human pathogens can respond to chemical signals from plants [4] and, from that perspective, human pathogens may share properties with other micro-organisms commonly present in plant microbiomes. From an evolutionary perspective, it make sense that particular groups of zoonotic species are able to use plants as secondary habitats. These microbes can be transferred via feces among different flocks that graze on the same land [5]. Longer persistence on grazed plants may contribute to a wider distribution over different flocks. It is an important message for plant production that microbial interconnectivity will exist between ecosystems and that human pathogens can circulate between animals and plants when animal manure is applied to soil for fertilization [6]. Water used for irrigation is another human pathogen source in agricultural production systems, especially when derived from surface water bodies [7]. Human pathogens can contaminate surface water via drainage from arable fields recently fertilized with animal manure [8], but also from sewage overflow after severe precipitation [9] and wildlife [10].
The contamination of plant-derived products with human pathogens thus does not only result from harvest and post-harvest handlings, but can also occur at the primary production stage. The network activities of the EU COST Action on the control of human pathogens in plant production systems (HUPLANTcontrol) comprehended important aspects that were intended to gain a better understanding on the role of human pathogens in plant microbiomes in relation to ecology, taxonomical identity, and presumed virulence to humans. This information was relevant for the formulation of recommendations and guidelines to growers, but also to provide public information on the consequences of the presence of human pathogens in plant production systems. This Special Issue was dedicated to the main objectives of our network activities and resulted in seven manuscripts that are related to the topic of human pathogens in their relationship with plants.
It was shown that Escherichia coli, introduced via manure and seeds in production systems, had a higher preference for the root zone (roots and rhizosphere soil) than for the above-soil compartments [11,12]. Although different E. coli strains were incidentally found in stem parts shortly after their introduction, their abundance rapidly declined to levels below detection, whereas near, on, and inside roots, the introduced strains remained present up to plant senescence. As both experiments were performed under field-realistic circumstances, the key message derived from both manuscripts is critical for practice, because it would imply that plant roots are potential carriers of human pathogens once they are disseminated into production systems via external sources. The ability for microbial species to jump over from plant to animal kingdoms was indicated for two taxonomically distinct micro-organisms, Fusarium musae [13] and Bacillus cereus [14]. Namely, F. musae strains with the same genetic profile could infect both humans and plants (banana fruit), whereas B. cereus strains derived from 17 different agricultural soils sampled across Europe possessed genes that are potentially involved in human pathogenicity. Both studies made clear that human pathogens in plant production systems do not necessarily originate from external sources, but can be intrinsic members of soil and plant ecosystems. Soil treatment with composted sewage sludge resulted in a shift in the soil microbiome composition [15]. Salmonella enterica survived longer when simultaneously applied with composted sewage sludge to soil than when applied separately via irrigation. Changes in microbiomes as a result of soil amendments may thus influence the persistence of human pathogens in food production soils, and this information is relevant for understanding the mechanisms behind the soil persistence of human pathogens. Finally, it revealed that plants themselves can influence the behavior of human pathogens. Upon plant inoculation, flagellin expression was down-regulated in a vast majority of S. enterica cells, whereas high expression was found in a subfraction of the introduced population [16]. Heterogenous flagellin expression is an adaptational strategy of S. enterica inside plants. Plants defend themselves upon colonization by human pathogens via activating defensive networks [17]. Bioactive compounds produced by plants antagonize human pathogens in plants, offering new opportunities for the control of human pathogens in plant production systems.
The seven manuscripts in this Special Issue provide new and important information on the ecological behavior of human pathogens in the plant–soil environment and the roles that microbiomes play. They also demonstrated that plant microbiomes themselves harbor species that can potentially cross plant–animal frontiers and that the plant environment is a specific ecosystem where human pathogens are able to adapt to local prevailing circumstances. Valuable information was provided for further translation into practical recommendations, which is needed for the control of human pathogens in, or nearby, growing plants. Finally, the information provided is relevant for the transition towards extensive and circular agricultural production systems. The use of animal manure and other organic waste streams and reclaimed water as alternatives for fertilizers and irrigation water will become more opportune in this transition, affecting the introduction of human pathogens into plant production systems.
Posted in Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, Fumomisins, Fumonsins, Fusarium Toxin, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Pathogen, pathogenic, Salmonella
USA – Canned Shrimp recalled due to Botulism risk
Kawasho Foods USA Inc. of New York, NY, is voluntarily recalling one lot of canned GEISHA Medium Shrimp 4oz. because of reported swelling, leaking, or bursting cans. There is a possibility that the product has been under processed, which could lead to the potential for spoilage organisms or pathogens.
The Product was distributed to retail stores (Walmart, Associated Food Stores, Stater Bros Markets, Safeway, Albertsons) in California, Utah, Arizona, and Colorado.
The GEISHA Medium Shrimp is packaged in a 4oz. metal can, with UPC 071140003909. The one lot being recalled is LGC12W12E22; BEST BY: MAY/12/2026 and this code appears on the bottom of the product can.
Posted in Clostridium, Clostridium botulinum, Clostridium Sulphite Reducer, food contamination, food handler, Food Hazard, Food Hygiene, Food Inspections, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Testing, Food Pathogen, Food Poisoning, Food Quality, food recall, Food Safety, Food Safety Alert, Food Safety Management, Food Safety Regulations, food safety training, Food Spoilage, Food Testing, Food Toxin, Pathogen, pathogenic
USA – Kawasho Foods USA Inc. Announces a Voluntary Recall of a Single Lot of GEISHA Medium Shrimp 4oz. Because of Possible Health Risk

Company Announcement
Kawasho Foods USA Inc. of New York, NY, is voluntarily recalling one lot of canned GEISHA Medium Shrimp 4oz. because of reported swelling, leaking, or bursting cans. There is a possibility that the product has been under processed, which could lead to the potential for spoilage organisms or pathogens.
The Product was distributed to retail stores (Walmart, Associated Food Stores, Stater Bros Markets, Safeway, Albertsons) in California, Utah, Arizona, and Colorado.
The GEISHA Medium Shrimp is packaged in a 4oz. metal can, with UPC 071140003909. The one lot being recalled is LGC12W12E22; BEST BY: MAY/12/2026 and this code appears on the bottom of the product can.
Consumers should not use this product, even if it does not look or smell spoiled. No illnesses or other adverse consequences have been reported to date in connection with this product.
Consumer who have purchased this product are urged to return to place of puchase for a full refund. If you have any question regarding this recall, please contact us at (212)841-7400 (Monday to Friday, 9:00 a.m. to 5 p.m. EST) or via email at info@geishabrand.com.
Posted in FDA, food contamination, food handler, Food Hazard, Food Hygiene, Food Inspections, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Pathogen, Food Quality, food recall, Food Safety, Food Safety Alert, Food Safety Management, Food Safety Regulations, Food Spoilage, Food Testing, Pathogen, pathogenic
Research – Presence and Persistence of Listeria monocytogenes in the Danish Ready-to-Eat Food Production Environment
Abstract
Listeria monocytogenes is an ubiquitously occurring foodborne bacterial pathogen known to contaminate foods during the production processes. To assess the presence and persistence of L. monocytogenes in Danish ready-to-eat (RTE) food production companies in response to a Listeria awareness campaign, the production environment of selected companies were sampled in 2016 and in 2020. Whole genome sequencing (WGS) was performed to characterize the isolates (n = 50, plus 35 isolates obtained from the routine surveillance during 2016–2020), including investigation of the presence of virulence, persistence and resistance genes. The number of companies that tested positive by culture was 17/39 (43.6%) in 2016 and 11/34 (32.4%) in 2020, indicating a limited effect of the campaign. WGS analyses of the 85 isolates showed that the most common sequence types (STs) were ST8 and ST121. The single nucleotide polymorphism (SNP) analysis showed that isolates coming from the same company and belonging to the same ST exhibited <10 SNP differences regardless of the sampling year and whether the samples came from the environment or products, indicating the persistence of the specific STs. Several prevalent STs were found in clinical cases concurrently, including genetically similar isolates. This highlights the issue of persistent L. monocytogenes in the food production environment and the need for improved risk communication and mitigation strategies.
Posted in Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, Listeria, Listeria monocytogenes, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Pathogen, pathogenic
Research – E. coli, Salmonella, and Campylobacter: How Important is Sanitizing Your Shopping Cart?
During the height of the pandemic, grocery stores began routinely sanitizing shopping carts and baskets after each use to reduce the spread of the COVID-19 virus. Now that the rate of COVID infections is far less, this practice of cleaning carts is becoming a thing of the past. However, sanitizing shopping carts is extremely beneficial to minimize the spread of foodborne pathogens and grocery stores should not overlook its importance.
In a study by the University of Arizona, their results found that the number of bacteria on a shopping cart was higher than the amount on surfaces of a public restroom and on diaper changing stations because restrooms are frequently cleaned. Out of the 85 shopping carts tested, a remarkable 51% carried evidence of E. coli. Traces of salmonella and campylobacter were also found. These foodborne illness causing bacteria can all survive on surfaces for extended periods of time. Campylobacter can survive on a surface for up to 4 hours and Salmonella up to 32 hours. These types of bacteria can cause symptoms such as diarrhea, headache, fevers, and vomiting.
It is also very important to keep sanitation in mind when handling food in the grocery store that will not be reheated before consumption. Shoppers inevitably touch these foods immediately after manouvering the cart and risk spreading bacteria to the food they purchase.
Posted in Decontamination Microbial, Food Micro Blog, Food Microbiology, Food Microbiology Blog, Food Microbiology Research, Food Microbiology Testing, Food Pathogen, microbial contamination, Microbial growth, Microbiological Risk Assessment, Microbiology, Microbiology Investigations, Microbiology Risk, Pathogen, pathogenic

