MPI
New Zealand Food Safety is approaching its target to reduce rates of campylobacteriosis, the country’s most common foodborne illness, a new report published today has found.
Annual report concerning Foodborne Diseases in New Zealand 2023 [PDF, 5 MB]
The report, prepared for New Zealand Food Safety by the Institute for Environmental and Scientific Research (ESR), found that the rate of New Zealand-acquired foodborne illness caused by the bacteria Campylobacter has fallen from 88 to 77 cases per 100,000 population over the past 4 years.
“New Zealand Food Safety has made reducing campylobacteriosis rates a key priority, and we’ve made great strides in recent years,” says New Zealand Food Safety deputy director-general Vincent Arbuckle.
“Rates of infection more than halved between 2006 and 2020. In 2020 we set a target to reduce the rate by a further 20%, taking it to 70 cases per 100,000 by the end of 2024.
“These latest results show this goal is in sight, which is a testament to the combined and sustained work of government and industry over time.
“The Campylobacter Action Plan, put in place to help tackle the issue, mainly focuses on steps to reduce the levels of Campylobacter through the poultry food chain. We have worked with government, industry and NGOs right across the poultry food chain through the Campylobacter governance group with representatives from Ministry of Health, Poultry Industry Association of New Zealand, Foodstuffs North Island, Foodstuffs South Island, Woolworths NZ, and Consumer NZ.”
Campylobacter Action Plan
The poultry industry has continued to improve processing practices over time, resulting in a sustained reduction in the proportion of birds that have detectable levels of Campylobacter at the end of primary processing.
While changes in the food supply chain have achieved good results, consumer awareness remains an important part of the effort, Mr Arbuckle says.
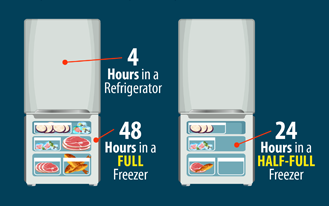
“We know that about half of all foodborne illness is caused at home. These illnesses can be prevented with good food preparation techniques as well as proper cooking and storage.
“To support prevention of Campylobacter at home we run public education campaigns which focus on giving people information they can use to keep themselves safe.
“While it is rewarding to see campylobacteriosis rates falling, there is more work to do. The symptoms of campylobacteriosis can be unpleasant for healthy adults and the consequences for the very young and people over 65 can be serious.”
The report also provides data on other foodborne illnesses in New Zealand, including listeriosis, which remains steady with 37 cases notified this year, Mr Arbuckle said.
“Listeria is common in the environment and while case of illness are low, listeriosis can have tragic consequences, including death. Of the notified cases, 26 people were in the 60-plus age group, and 7 people died with listeriosis this year.
“There are a range of practical measures people can take at home to reduce their risk from Listeria. More information is available on our website.
Listeria infection: symptoms and advice
New Zealand Food Safety ran a Listeria education campaign in June targeting pregnant people and those aged over 60.
By the numbers:
- 76.8 campylobacteriosis cases per 100,000 population, with 4,010 cases domestically acquired
- 989 hospitalised with campylobacteriosis, with 325 in the over-70 age group – the highest number of hospitalisations across all age groups
- 37 cases of listeriosis, with 7 deaths. 26 of these cases occurred in people aged over 60.
Media release: Simple steps to avoid life-threatening listeriosis
Campylobacter infection: symptoms and advice
For further information and general enquiries, call MPI on 0800 00 83 33 or email info@mpi.govt.nz
For media enquiries, contact the media team on 029 894 0328.