FDA
Do not eat, sell, or serve recalled organic walnuts sold in bulk bins at natural food and co-op retailers in multiple states. FDA’s investigation is ongoing.

Product
Recalled organic walnut halves and pieces sold in bulk bins at natural food and co-op stores in AK, AR, AZ, CA, CO, HI, ID, KS, LA, MT, NE, NM, NV, OR, SD, TX, UT, WA, and WY. Some stores may repackage bulk walnut halves and pieces into plastic clamshells or bags.
FDA’s investigation is ongoing to determine if additional products or states are affected. This advisory will be updated as information becomes available.
Symptoms include severe stomach cramps, diarrhea, fever, nausea, and/or vomiting. Symptoms begin anywhere from a few days after consuming contaminated food or up to nine days later.
The severity or presence of certain symptoms may depend on the type of pathogenic E. coli that is causing the infection. Some infections can cause severe bloody diarrhea and lead to life-threatening conditions, such as a type of kidney failure called hemolytic uremic syndrome (HUS), or the development of high blood pressure, chronic kidney disease, and neurologic problems.
Stores Affected
Recalled organic walnut halves and pieces were sold in bulk bins at natural food and co-op stores in AK, AR, AZ, CA, CO, HI, ID, KS, LA, MT, NE, NM, NV, OR, SD, TX, UT, WA, and WY. A full list of store names and locations is available.
FDA is working with the firm and its distributors to determine whether additional store locations, products, or states are affected. FDA is sharing what is known at this time and will continue to update as more information is available.
Status
Ongoing
Recommendation
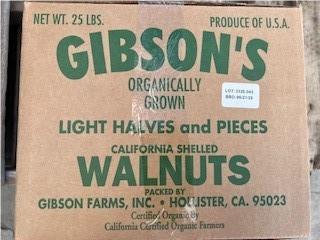
- Retailers and distributors that purchased recalled boxes of Gibson Farms, Inc. organic walnuts halves and pieces with lot codes 3325-043 and 3341-501 should not sell this product and should notify their customers of the recall. Product was shipped to distributors between the dates of October 1, 2023, to April 24, 2024. These products have expiration dates of 5/21/25 & 6/7/25.
- Retailers that have or had recalled product in bulk bins should discard the contents of the bins and use extra care to clean and sanitize the bins before refilling.
- Retailers that are unsure if they received recalled product may need to contact their supplier. If you are unable to determine whether or not recalled product was received, you should discard the contents of the bins and use extra care to clean and sanitize the bins before refilling.
- Consumers who purchased organic walnut halves and pieces from bulk bins at stores listed below should check their pantries, refrigerators, and freezers and should not eat the organic walnuts halves and pieces. If you have these products in your home, do not eat or use them, throw them away and clean and sanitize surfaces they touched.
- Retailers, distributors, and consumers should follow FDA’s safe handling and cleaning advice and use extra care in cleaning and sanitizing any surfaces and containers that may have come in contact with this product to reduce the risk of cross-contamination.
- Contact your healthcare provider if you think you may have symptoms of an E. coli infection after eating organic walnuts.
Case Counts
Total Illnesses: 12
Hospitalizations: 7
Deaths: 0
Last Illness Onset: April 4, 2024
States with Cases: CA, WA
Product Distribution*: AK, AR, AZ, CA, CO, HI, ID, KS, LA, MT, NE, NM, NV, OR, SD, TX, UT, WA, and WY