Certain live mussels from Allen’s Fisheries, Ltd. (NL0047SP), Benoit’s Cove, Newfoundland, Canada were initially harvested on 2/07/2024 (Julian date 24038) from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and shipped to distributors in CT, FL, MD, MA, NJ, NY, and PA on or around 2/21/2024 (Julian Date 24052). The live mussels were distributed to restaurants and retailers in CT, FL, MD, MA, NJ, NY, and PA and may have been distributed to other states, as well.
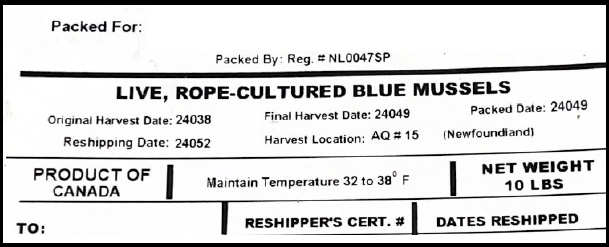
The following product tag is provided to be representative of labeling that would accompany the implicated mussels.
Purpose
The FDA is advising restaurants and food retailers not to serve or sell and to dispose of mussels and consumers not to eat mussels from Allen’s Fisheries (NL0047SP) in Newfoundland, Canada, harvested on 2/07/2024 (Julian date 24038), from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and shipped to distributors in CT, FL, MD, MA, NJ, NY, and PA on or around 2/21/2024 (Julian Date 24052) because they may be contaminated.
Contaminated shellfish can cause illness, especially if eaten raw, particularly in people with compromised immune systems. Food contaminated with pathogens or biotoxins may look, smell, and taste normal. Consumers of these products who are experiencing food poisoning symptoms such as diarrhea, stomach pain or cramps, nausea, vomiting, or fever should contact their healthcare provider, who should report their symptoms to their local Health Department.
Summary of Problem and Scope
On 3/1/2024, the New Jersey Department of Health advised the FDA of an outbreak of illness associated with consumption of certain mussels. The cases experienced symptoms including nausea, vomiting and diarrhea. The advisory includes mussels from Allen’s Fisheries (NL0047SP) in Newfoundland, Canada, harvested on 2/07/2024 (Julian date 24038), from harvest area AQ # 15 Newfoundland, with final harvest date of 2/18/2024 (Julian date 24049) and shipped to distributors in CT, FL, MD, MA, NJ, NY, and PA on or around 2/21/2024 (Julian Date 24052).